The Glasgow Coma Scale (GCS) is an evaluation tool used by neurologists and medical professionals to give a reliable, objective record of a patient’s conscious state as well as an initial assessment whenever a traumatic brain injury (TBI) is suspected or has occurred.
Glasgow Coma Scale Origins
The scale was first published by Graham Teasdale PhD, and Bryan J. Jennet, PhD in 1974, both professors of neurosurgery at the University of Glasgow’s (Scotland) Institute of Neurological Sciences at the city’s Southern General Hospital. The GCS was first used to assess patients’ level of consciousness following a head injury, but was quickly adopted by the medical industry and is clinically accepted by EMS workers, nurses, and doctors worldwide to evaluate trauma patients during triage, as well as those recovering in intensive care units.
Using the GCS
Any type of head injury may be detectable based on GCS evaluation results, and the assessment can be performed very quickly. Severe injuries, resulting in complete unconsciousness, typically receive the lowest score and typically prompt immediate surgical intervention. The following closed head injuries can also impact the GCS evaluation:
- Concussions
- Cerebral Contusions
- Intracranial Hematomas (Subdural/Epidural)
- Diffuse Axonal Injury
Understanding How Glasgow Coma Scale Works
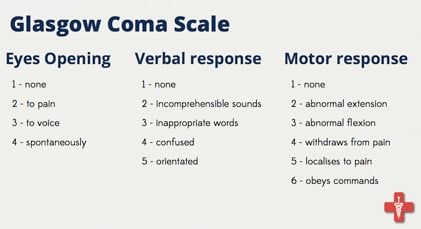
The scale is composed of three tests: Eye (E), Verbal (V) and Motor responses (M). Both the three independent scores and the total sum are considered separately in the patient’s assessment.
Eye Response (4-Best Score):
- No eye opening
- Eye opening to pain
- Eye opening to verbal command (in response to a command, not awakening from sleep)
- Eyes open spontaneously
Verbal Response (5-Best score):
- No verbal response
- Incomprehensible sounds (moaning, not words)
- Inappropriate words (comprehensible exclamations, non-relevant or non-conversational sentences or statements)
- Confused (able to answer questions with coherence, but may experience short-term memory loss or disorientation, unaware of injury occurrence)
- Orientated (patient is fully coherent, understands why/where they are)
Best Motor Response (6-Best Score):
- No motor response
- Extension to pain (arm abduction, supination of forearm)
- Abnormal flexion to pain (pronation of forearm, flexor posturing)
- Withdrawal from pain (pulls away from pain source – pulls hand away when fingernails are pinched)
- Localizing pain (purposeful movement toward pain – patient holds/touches head with severe headache or pain)
- Obeys Commands (patient can execute simple commands with ease)
GCS Score Translation
Medical staff and doctors must account for individual elements and the sum, so GCS results are coded with the time of day as such:
GCS 8 = E2 V3 M3 at 13:24.
Early brain injury assessment is then categorized as:
- Severe: GCS < 9
- Moderate: GCS 9 to 12
- Mild/Moderate: GDC ≥ 13
Diagnosis and treatment plans are typically based on the outcome of further scans and testing.
References:
UNC – Chapel Hill